(This is Part 26 of Dr. Pagtakhan's column, Medisina at Politika, on Covid 19.)
[Ed’s Note: In February 2020, CFNet started publishing Dr. Rey Pagtakhan’s column, Medisina at Politika, on COVID-19. Now on Part 26 of his running commentary, Dr. Pagtakhan’s twice a month column has kept the Filipino community and other CFNet readers continually informed about 1) the pandemic and its impact, 2) the scientific advances on drugs and vaccines, and 3) the effectiveness of public health responses, including mass vaccination as a vital step to individual protection and development of herd immunity (also called community or population immunity).]
“Variants of concern increase the threat for a spring resurgence,
but a strong collective effort can see us through.
With a combination of strong public health measures
AND
strict adherence to individual precautions,
we can prevent a resurgence.” - PHAC, February 19th, 2021
On February 19, the Public Health Agency of Canada released its Report, Update on COVID-19 in Canada: Epidemiology and Modelling, which conveys the above-noted warning forecast. Taking into account the emergence of new SARSCoV-2 variants of concern (VOC) and the current public health measures (PHM) in place in provinces and territories, the Report gives the following projections:
- If PHM are prematurely lifted, the VOC would trigger a pan-Canadian resurgence so rapid as to create a third wave akin to the most lethal pandemic curve of the Spanish flu a century ago;
- If PHM are kept at the same level or loosen, VOC would also cause a third-wave resurgence, although not as rapid, before more intense rapid mass vaccination starts in April; and
- If PHM and individual compliance are combined and made more stringent and stricter, resurgence would be prevented and control of the epidemic would be achieved, that is, the country will avoid a third wave.
Based on the average daily new case counts of 2,886 the week preceding the Report, Canada’s top public health expert Dr. Theresa Tam elaborated on the modelling projections, using actual numbers and assuming the new VOC are 50-per-cent more transmissible than the current dominant form of COVID-19 virus in Canada (Marieke Walsh: Globe and Mail.Feb.19, 2021):
- If the current restrictions remain in place, Canada could see 10,000 cases a day by the end of March;
- If these restrictions are lifted, Canada could be on track for more than 20,000 daily new cases by mid-March.
Using the same assumption for transmissibility of the variants, the U.S. Centers for Disease Control and Prevention conveyed a similar message with its own forecast published five days later (Christina Maxouris: CNN. Feb.25).
Indeed, one shudders at the likelihood of a pandemic third wave. This is particularly gnawing in light of the observations during the last couple of months that overall new cases, hospitalizations and deaths in Canada and in the world, including in the epicenter U.S.A., have seen a decline. While the downward trend could be due to mass vaccination that started in December 2020, to better adherence with stricter public health measures, to supportive and coordinated political leadership, or to any combination of these factors and, therefore, we could not be definitive which factor(s) played the beneficient role. the flattening of the curve that has been observed this past week may reflect the adverse influence of the new virus variants. If so, the earlier progress that has been made is once more under threat.
Are we seeing the early signs of pandemic resurgence - the third-wave pandemic storm after a calm of progress? To not make it inevitable, we are well advised to follow public health guidance and do our individual best to have (Public Health Agency of Canada. February 19th, 2021): “the FEWEST interactions, with the FEWEST people, for the SHORTEST time, at GREATEST distance possible, while wearing the best-fitting face-mask.”
SARSCoV-2 Variants of Concern (VOC)
Canada has to date identified across all 10 provinces 976 COVID-19 cases with SARSCoV-2 VOC, most notably the following, with B.1.17 being the most dominant type:
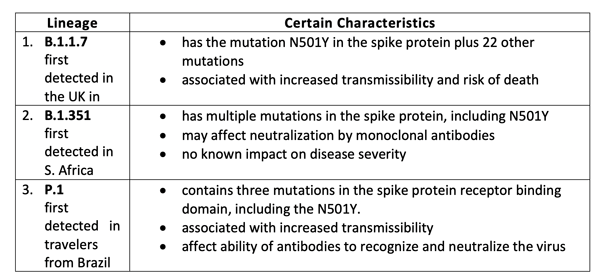
The above-noted three variants each has the N501Y mutation associated with increased transmissibility, severity of disease, and death. The VOC have one or more mutations that differentiate them from the wild-type or predominant virus variants already circulating among the general population, which contain no major mutation. A common characteristic among the VOC is the role of international travels in transmission. Three of the five cases recently detected in Manitoba were related to international travel.
In the U.S., more than 1,900 of the three major variants seen in Canada have also been identified, almost all of which belong to the B.1.1.7 lineage. Two forthcoming reports from California on new variants, B.1.427/B.1.429, which are associated with severe infectiousness and severity, are soon to be published (Ivana Kottasová: CNN.Feb 24).
What exactly are the concerns about the new SARSCoV-2 variants?
That these VOC may have the following characteristics (U.S. Centers for Disease Control and Prevention):
- Ability to evade natural or vaccine-induced immunity - Both natural infection with and vaccination against SARS-CoV-2 produce a “polyclonal” antibody response that targets several parts of the spike protein. The virus could accumulate significant mutations in the spike protein to evade immunity induced. This is the most worrisome concern since Canada and the other countries have only begun their vaccination drive barely two months ago and the percent of the population who had been fully vaccinated is nowhere near the level required to establish herd immunity.
- Ability to spread more quickly in people - One study has shown transmissibility increased by about 50%, which would most certainly increase the number of cases in the community.
- Ability to cause either milder or more severe disease in people - If the increase in caseload is accompanied by serious cases requiring oxygen therapy and ventilator-assisted breathing, the acute care burden can overwhelm the health system once more. Preliminary studies have shown predisposition of some VOC to cause more severe disease requiring oxygen therapy.
- Ability to evade detection by specific diagnostic tests – Many diagnostic tests use multiple targets to detect the virus, hence, would still work even if a mutation impacts one of the targets. Tests that rely on only one target may fail in their diagnostic capability. This is being closely monitored.
- Decreased susceptibility to therapeutics that employ monoclonal antibodies - These treatments are more specific than natural immune response-generated antibodies; hence, they may be less effective against variants that emerge.
How do variants occur?
Basically, a virus variant is the natural consequence of replication that occurs in a virus’ life history in the human host over time.
Viruses such as SARS-CoV-2, the virus that causes COVID-19, are constantly changing. The virus genome packed inside an envelope contains proteins and instructions to build parts of the virus, for example, the spike protein, which allows the virus to attach to human cells during a human infection. This section of the genome serves as a key region for monitoring mutations. Mutations are changes in the genetic code of a virus that naturally occur when a person is infected. A certain amount of genetic variation is expected to occur over time. While many of them do not affect the virus’s ability to spread or cause disease because they do not alter the major proteins involved in an infection, it is crucial to monitor circulating viruses for key mutation(s) that happen in important regions of the genome for the variants with mutations that are more beneficial for the virus.
Dr. Alyson Kelvin, a Canadian virologist and researcher in vaccine development, in a recent news interview (Lauren Pelley. CBC News. Jan 19, 2021), said it this way: “Each virus has a singular goal of replicating itself. With tens of millions of people helping move the coronavirus back and forth between hosts, that means countless replications. Some of those contain random, insignificant mistakes. And when the mistakes prove beneficial to the virus, helping it produce more copies, those errors can become a new normal of sorts – a variant.”
Understanding better the singular goal of a virus – sharing a recent reading
Last month’s edition of the National Geographic magazine (February 2021, Volume 238, No.2) is dedicated to the Mysteries of a Virus – as the title printed on the front Cover with the image of the Mimivirus in the foreground aptly displays. (Note: Scientists anticipate that studying this virus – “one of the largest and most complex viruses known will shed light on viruses’ origins and proliferation.”)
The magazine’s lead article, ‘How Viruses Shape Our World’ by David Quammen timely caught my attention as I thought over the theme for my Commentary. His essay attracted my curiosity not only for the ample illustrations provided by the artist and photographer Craig Cutler “to tell a story in each image,” but also for the author’s narration of the subject matter that makes it so instructive as to help clarify for me a teaching in virology I first heard during my medical school days, that is: 1) a virus is inanimate, which means it is destitute of life, and 2) a virus wants to replicate – to copy itself – which means it is animated and implies the presence of functional activity.
This teaching, when presented simply in this manner – the first independent from the second – has since posed a seeming puzzle to me, intermittently over the years. Following a reading of his essay, I thought I should share a brief of his insights as a supplement to the theme of this present Commentary.
Virions and virocell – delineating the inanimate and the animated parts of a virus
t is to the above-noted seeming conundrum that Quammen’s exposition led me to focus on the behaviour of a virus when residing inside the human host and exercising its inherent mandate, or residing outside the human cell, suspended in the air as aerosol or lying on surfaces as fomites, waiting to enter the human cell at the first opportunity. He quoted in his essay scientist Patrick Forterre of the Pasteur Institute in Paris, France who explained: “Scientists were confusing the viral particles known as virions (the bits of genome or genetic material enclosed in a protein coat or shell or envelope) with the totality of a virus, and was as wrong as confusing a seed with a plant.”
The French scientist went on to further explain that the virions, which are inanimate, are only a part of the totality of a virus. “The real wholeness of the virus,” he continued, “also includes its presence within a cell, once it has seized the cell’s machinery to replicate more virions, more seeds of itself.” When that has happened, “the cell has become part of the virus’s life history.”
For this combined entity, he coined the new term, ‘virocell.’ In this stage as it happens when a virus infects a person, the wholeness of the virus is expressed and active, not inanimate, and obeys the official viral mandate, that is, “reading the viral genome and replicating it.” That is the wholeness of the virus complying with its inherent domain or natural property – to replicate itself.
The pathogenic virus SARSCoV-2 that causes COVID-19 is a single-stranded RNA virus. As such, its RNA genome is prone to undergo, over time, mutations or variations as the virus replicates to make more viruses. The opportunity to replicate its genome occurs whenever the virus infects people and resides in their cells. And every time it replicates its genome, chances for “skips, staggers, and mistakes” – errors or mutations – are bound to happen, notwithstanding it has proofreading enzymes to correct most of the mutations.
For a little over a year now since it first infected a cluster of citizens in Wuhan, China in early December 2019, SARSCoV-2 has been globe-trotting in the comfort of its human host. In the first few human hosts infected, we have learned the virus replicated in abundance, harmed body organs primarily the lungs, and soon managed to spread – human to human - across the country and across continents.
Until now, it continues to encircle the world, leaving in its path misery of illness and deaths to millions of the world citizens. It needs little imagination to acknowledge that the viral genome has been replicated billions of times. Intuitively during this period of time, errors must have been incorporated, resulting in many new variants with mutations on certain regions of the viral genome of the original, wild-type circulating SARSCoV-2 which had with very few mutations and none major.
Sadly, the human cell – the human host - has become part and parcel of the COVID-19 virus’ life history and travels. Fortunately, we have the vaccines and the proven public health measures to stop its global journey. We shall not allow a pandemic third wave after the calm.
 A Montreal surfer rides a wave on the St. Lawrence River on Jan. 18. Experts say despite a decline in COVID-19 cases nationally, variants threaten to spark a third wave of the pandemic that might be more devastating and harder to control. (Credit: CBC/Radio-Canada; Adam Miller: CBC News, Feb 24, 2021)
A Montreal surfer rides a wave on the St. Lawrence River on Jan. 18. Experts say despite a decline in COVID-19 cases nationally, variants threaten to spark a third wave of the pandemic that might be more devastating and harder to control. (Credit: CBC/Radio-Canada; Adam Miller: CBC News, Feb 24, 2021)
[P.S: As of Feb. 25 per Johns Hopkins University Coronavirus Tracker, the global total cases and deaths are, respectively = 112,999,297 and 2,507,444; Canada’s burden = 863,495 and 21,868; U.S.A.’s = 28,411,273 and 508,127; and the Philippines’ = 568,680 and 12,207, respectively.]